COVID-19 has put a significant strain on healthcare systems in Asia and around the world. With the outbreak of the pandemic and the surge in the number of patients requiring beds for COVID-19 response, many hospitals in the region have had to shift resources away from any non-intensive ICU treatments.1 This has led to the temporary closure of many so-called ‘elective’ treatments, including testing for chronic obstructive pulmonary disease (COPD) as well as services for patients with sleep disorders.
As the word ‘elective’ implies optional, this has created a complex situation for respiratory specialists responsible for the management of the COPD patient population during this pandemic. According to a recent article in the European Respiratory Journal, we have not yet quantified how many COPD patients may have chosen, or were unable to, visit hospitals during this pandemic.2 Although researchers hypothesise—drawing on learnings from the previous SARS epidemic, where chronic disease patients not affected by SARS ‘presented with worsened disease/symptom control’ largely attributed to ‘a widespread avoidance of the health care system’—that a similar situation is likely occurring in the COVID-19 pandemic.3
According to the Global Burden of Diseases (GBD) Study 2017, there were 3.2 million deaths due to Chronic Obstructive Pulmonary Disease (COPD) and 495 thousand deaths due to asthma.4 In Asia, the estimated prevalence of COPD in the region is rising according to Asia Pacific Family Medicine. However, the disease has historically been under-diagnosed and under-reported even before the outbreak of COVID-19.5 This situation will likely be exacerbated as health systems move towards recovery due to overburdened hospitals with backlogged cases and where spirometry cannot be performed.
The first reality that hospital leaders now face is the huge backlog of respiratory service cases caused by the closure of all non-critical services during the peak of the pandemic. However, even now despite this backlog and services reopening, volumes remain low. For example, South Korea and Thailand hospitals were conducting as low as 40 percent volume of elective/semi-elective procedures as of last month.6
A primary reason for this low volume could be patients’ concern over safe care environment and risk of infection when seeking so-called ‘elective’ services. Given the devastating impact that COVID-19 can have on the lung, it is natural for patients with underlying COPD to avoid hospitals during this time.7
“Even though some services have restarted, patients are quite concerned about hygiene in a hospital setting,” said Prof. Susanna Ng of the Department of Medicine & Therapeutics Faculty of Medicine, The Chinese University of Hong Kong in a recent interview with ResMed.
Such fears can lead to further delays in administering proper care, which can culminate in lasting impact on health.
Hospital administrators are striving to ensure patients of hygiene so that they are more likely to access necessary treatments, while also taking measures to protect the long-term wellness and safety of their staff. Minimising potential exposure to infection and creating a safe environment during the pandemic is top of mind. This has caused many administrators to re-examine some standard practices as they begin their post-pandemic planning.
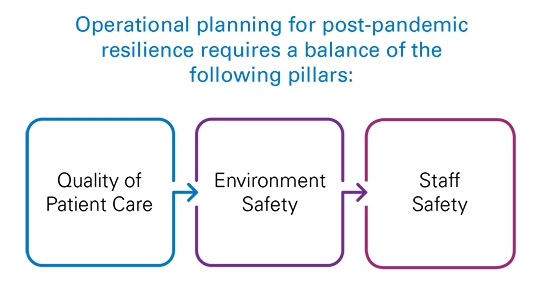
Quality of Patient Care
Many hospitals are facing a huge backlog of uncompleted procedures due to the various policies during the height of the pandemic. A wealth of literature points to negative patient outcomes and higher costs when certain treatments are delayed.8 It is important that hospitals are leveraging all technologies at their disposal to start bridging these gaps early.
Environment Safety
The pandemic has exacerbated longstanding public health and environmental challenges, requiring administrators to balance the need for staff safety against impacts to the environment.9 The crisis will require a careful balance of both reusables and disposables to ensure that they are minimising exposure to infection.
Staff Safety
At least 72,346 US healthcare workers have been infected during this pandemic as of June 4, 2020.10 Countless more healthcare workers are exposed to infection around the world, spurring the Harvard Business Review to implore administrators to re-examine their practices to ‘make staff safety a fundamental value that you won’t compromise for other organisational priorities.’11
For example, many hospitals in Asia that perform in-patient testing for respiratory patients, still rely on reusable masks for cost efficiencies.
A recent paper12 lead by Dr. Ken Junyang Goh, Department of Respiratory and Critical Care Medicine, Singapore General Hospital, and Dr. Jolin Wong, Division of Anaesthesiology, Singapore General Hospital, discusses practical considerations in hospital planning during and after COVID-19. The authors advise that whenever staff are utilising reusable items it is of utmost importance to ‘ensure adequate capacity for prompt disinfection and sterilisation’ and that in some cases of infection control where facilities and manpower are strained ‘single use items may be preferable.’ Proper disinfection and sterilisation processes of CPAP and NIV masks used in clinic settings require staff follow specific disinfection protocols or specially approved sterilisation machines. The need to minimise healthcare workers’ exposure to potential infections has driven several hospitals to consider stocking on disposable masks, in addition to reusable supply as a precautionary measure.
While both reusable and disposable variants have their roles respectively, the rising attention to minimise staff exposure to infection and patient preference are driving facilities to equip themselves with adequate supplies of both. In addition to ensuring availability of disposable masks in clinic, administrators are also considering supplying disposable accessories to accompany ventilation systems, such as disposable anti-bacterial filters, to mitigate exposure to both staff and patients.

AcuCare is one type of disposable mask, designed to achieve fast patient acceptance of noninvasive ventilation (NIV). By helping patients accept NIV quickly and successfully, healthcare providers can reduce the need for intubation, decrease the risk of infection, and reduce the cost and length of patients’ hospital stay.13
In addition to making preparations to minimise infection risk in a hospital setting, there are also new considerations for respiratory patients who are able to avoid hospital visits entirely, but still need support in managing their conditions during this pandemic. Administrators are paying attention to the shift in adopting technologies to empower patients to take charge of their own health. Such innovations may also help in reducing the burden on hospital facilities and healthcare workers as well as for carers at home.
“Through the pandemic, many rules around telehealth have been relaxed but this is not a problem. You can certainly avoid infection risk with virtual care, it’s much easier to reach out to a patient without travel issues,” said Dr. Patrick Strollo, Professor of Medicine and Clinical & Translational Science in the University of Pittsburgh’s division of Pulmonary, Allergy and Critical Care in an interview with ResMed.
There are several technologies that hospitals are considering for non-dependent patients with obstructive or restrictive respiratory conditions. For example, certain noninvasive ventilator systems such as Lumis 150 VPAP ST are designed to continuously monitor and support both the upper airway and alveolar ventilation from the comfort and safety of a patient’s home. Healthcare providers serving respiratory patients with reservations about visiting clinics may find such technology to be a viable alternative to ensure continued care while minimising infection risks.
Knowing the options available and empowering patients through technology can support continuity of care in out of hospital settings during this period.
The burden caused by COVID-19 to hospital systems in Asia is beginning to cause small but significant shifts in our care delivery. In light of this changing landscape, healthcare leaders need to understand the technology and tools available to help the ecosystem stay on top in infection control, and continue to deliver quality care for respiratory patients.
References:
1. Oliver Wyman. COVID-19: Responses & Implications to Healthcare in Asia. https://www.oliverwyman.com/content/dam/oliver-wyman/v2/publications/2020/apr/covid-asia-implications/COVID-19-Responses-and-Implications-To-Healthcare-In-Asia.pdf
2. To, Teresa. Viegi, Giovanna. Cruz, Alvaro, et al. A Global Respiratory Perspective on the COVID-19 Pandemic: Commentary and Action Proposals. European Respiratory Journal 2020. https://erj.ersjournals.com/content/early/2020/06/08/13993003.01704-2020
3. Ibid
4. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392: 1789–1858. doi:10.1016/S0140-6736(18)32279-7
5. Lim, S., Lam, D.C., Muttalif, A.R. et al. Impact of chronic obstructive pulmonary disease (COPD) in the Asia-Pacific region: the EPIC Asia population-based survey. Asia Pac Fam Med 14, 4 (2015). https://doi.org/10.1186/
6. https://www.healthcareitnews.com/news/asia-pacific/impact-COVID-19-apac-hospitals
7. To, Teresa. Viegi, Giovanna. Cruz, Alvaro, et al. A Global Respiratory Perspective on the COVID-19 Pandemic: Commentary and Action Proposals. European Respiratory Journal 2020.
8. https://hbr.org/2020/08/covid-19-created-an-elective-surgery-backlog-how-can-hospitals-get-back-on-track
9. https://www.eco-business.com/opinion/innovating-for-impact-dealing-with-a-mountain-of-medical-waste/
10. https://hbr.org/2020/06/health-care-workers-protect-us-its-time-to-protect-them
11. Ibid
12. https://link.springer.com/content/pdf/10.1186/s13054-020-02916-4.pdf
13. Lindenauer PK et al. Outcomes associated with invasive and noninvasive ventilation among patients hospitalized with exacerbations of chronic obstructive pulmonary disease. JAMA Intern Med. 2014 Dec 1;174(12):1982–93