COVID-19 has accelerated the pace of healthcare innovation and potentially extended how medical care is delivered. While these solutions hold incredible promises, we are adding more variables to variation in care. The future of healthcare should be driven by knowledge to deliver optimal care with patient safety and quality considerations.
Innovation in digital health has become a by-product of our collective healthcare experience through the COVID-19 pandemic. Since the onset of the pandemic, we have seen an explosion in innovation in the digital health space. Many countries in Asia, including China, Singapore, and Australia, were the first to experiment and roll out contact tracing mobile applications to step up preventive measures . In some regions, including South Korea, the government has also temporarily relaxed restrictions on telemedicine consultations to allow physicians to conduct remote diagnosis and monitoring . More recently, experts are racing to deploy other digital solutions to flatten the curve and recalibrate societies back to normal. What is more likely to be true is the realignment towards a new reality.
While these new solutions and technologies hold incredible promise, there are potential quality and safety considerations that need to be thoroughly examined. It is equally important to consider the impact and optimisation of the user experience, for both clinicians and patients.

Patients, clinicians, and health system funders realised that the old model of healthcare did not hold up well to the challenges and continuing evolving needs introduced by COVID-19. Technologists and entrepreneurs do what they do best; their creative and enterprising minds think of ways in which technology can address the myriad of challenges and barriers that have been identified. Find and identify the problem; solve it is the mantra. Telemedicine will solve the access constraint; apps can solve x, y, z; big data, artificial intelligence and machine learning will produce all this new knowledge and insights for clinicians. And the new normal is going to achieve a new state of equilibrium.
The risk of this kind of innovation approach is that we may think we have arrived at a solution, but really the solution addresses only one piece of the care puzzle. We may be introducing other problems or unintentionally pushing the pain point for clinicians, the consumer/patients or both somewhere else. The common analogy is what happens when you just squeeze one part of a balloon; the other sections naturally expand and will experience additional strain. Any introduction of new technology should streamline the entire process, and produce a positive and impactful experience for all stakeholders.
The future of healthcare will be a more Knowledge-driven Care Process.
What does this mean in tangible terms applied to healthcare digitalisation and innovation? Basically, healthcare delivery and what patients should expect is a level of care and consistency that aligns with the latest body of evidence-based knowledge and best practice standards, delivered via an optimised consumer-centred experience that is efficient, and cost-effective. A digital system to enable this vision is the basis of this proposed knowledge-driven care framework. Whatever technology we bring forth and however we transform healthcare delivery, it must align towards a knowledgedriven care process.
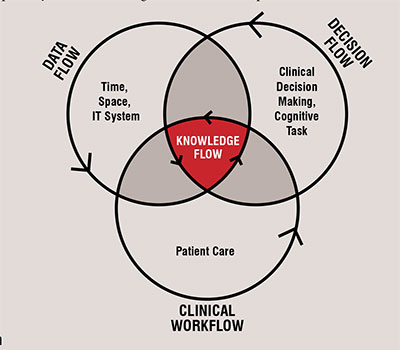
In order to enable knowledge-driven care, there are three intersecting dimensions (Clinical Workflow, Decision Flow and Data Flow) to consider, which are required to optimally deliver knowledge flow across a care process.
Clinical care is a series of complex, multi-disciplinary process that often cross clinicians and organisations, geography and time through the care continuum. Each step in the workflow has different contextual needs for data to support work and decision making. Whether it is electronic medical record (EMR) functionality or apps, making sure the technology clearly supports and if possible, improves the clinician’s workflow which is so important. There are too many experiences in which the technology is adding stress for clinicians and creating a barrier between the important human connection of the clinicians with the patients.
Along the workflow for a care process, many clinical decisions are made by clinicians. These decisions take place in the context of the clinical work and activities. Technology that aids the clinicians with this cognitive work such as clinical decision support (CDS) should smartly know what information is needed to make the best decisions; what decisions regarding care and treatment are important. Care should be coordinated across the care continuum and across clinicians; ideally all the decisions should be aligned to a common basis of knowledge, evidence and best practice targeting a common set of outcomes.
Key to knowledge is the availability of quality, machine interpretable data for easy access by clinicians and patients, and leveraged for decision support. Often, we assume the data is there. This passive mindset assumes that the important data to support clinical workflow and decision-making are accessible, reliable and computable. It takes planning and data architecture to ensure this. If there is a reliance on the use of specific data, then effort must be taken to ensure that i) the technology respect and handles the required data focused on validity, veracity, and ii) the clinical process sources the data in ways that will lead to usability of the data for clinical decision support.

What does it take to truly enable a knowledge driven care process? Because care takes place across time, involving different places and people, the key to the knowledge driven care process is the ability to support Knowledge Flow in the digital healthcare ecosystem.
Knowledge flow as the name implies, is how the right knowledge can be accessible throughout the care continuum, by the right individuals to make optimal treatment and care decisions to achieve the desired outcomes. With the new, foreseeable digital innovation and design of the new normal for healthcare delivery, considerations to each dimension of the knowledge flow is necessary to be successful and effective in achieving true knowledge-driven care. Basically, as an integrated framework, the flow of knowledge is achieved when the digital system supports the optimised clinical care activities (i.e. clinical workflow) based on sound and coordinated clinical decision making across the entire care process (i.e. the flow of decisions), and taps the right data necessary to support care and clinical decision making (i.e. data flow).
Fundamentally, we must appreciate and optimise how care is delivered, the important clinical decisions that must be made to guide clinical care, and the relevant information when or where it is necessary to support the clinical work and decisions. All three dimensions intersect to optimise how the most current and relevant evidencebased knowledge can flow and achieve the goals we desire, at the point of clinical action. Without simultaneous consideration and optimisation of all three dimensions, in the aggregate, there will be a lack of a cohesive process, and the physician-patient experience will not be ideal.
Fortunately, if we approach technology and the digitalisation of healthcare with human-centred design thinking, knowledge can be made accessible where and when healthcare professionals need it in a logical and utilitarian way. Clinical decisions and actions are made easier and more transparent through tools such as Clinical Decision Support (CDS) that design and manage machine computable data and factors in the clinician workflow in the design and system integration.
Conclusion
The road is littered with the casualties of experiences where technology was just thrown in as the answer to a problem. In providing a specific capability or solving a targeted problem area, the unintended consequences can include negative user experience, confusing data and information, or not achieving the desired outcome and possibly risk of safety and quality issues. As we continue riding the incoming waves of the pandemic with a new pace of innovation adoption, we must not overlook the need to ensure the flow of knowledge actually aids the clinician in a positive way and to ensure that patients continue to receive a level of care and consistency that puts patient safety and quality at the forefront.