Diagnosis is often difficult in the remote unreached communities with no access to professional pathologists although it is fundamental to provide appropriate treatment. During the Coronavirus (COVID-19) pandemic, it has become more important to accommodate innovative technologies of digital imaging and telecommunications for remote primary diagnosis, specialist referrals, research, and educational purposes. In this paper, we present recent progress in the research of telepathology in Bangladesh.
Telepathology can be explained as the electronic transmission of digital images of pathology for education, research, diagnosis, or consultation. The term ‘telepathology’ was invented in a scientific article by a pathologist Dr Ronald S Weinstein in 1986, who is also recognised as the ‘father of telepathology’. Using the internet and advanced telecommunication to provide remote diagnosis service is known as telepathology. The research of telepathology raised up and involving different field of research, education and using artificial in tendency. Currently, many countries have endeavoured to the analysis of research in telepathology for different poorhouses and beginning from the materials supplied by bibliometrics.
In the early 1950s, telepathology was developed from video microscopy (i.e., Television Microscopy) research to video microscopy used in basic research in the biological sciences. In 2011, during a multinational telepathology conference in Venice, Italy, the 25th anniversary of the publication of the first telepathology article (an editorial) in 1986 was marked and noted by Vincente Della Mea. A wide variety of digital slide imaging devices was demonstrated by twenty imaging companies. However, none of them were interoperable. The standards of telepathology were either nonexistent or at an early stage of evolution at the time of this multinational conference. Afterwards, although, more than 400 laboratories in 32 countries have published telepathology articles, proportionately few of them use telepathology in their practices apart from transformation of irregular intraoperative frozen section diagnosis or second opinions on problematic surgical pathology. For the surgical pathology cases, by using the realtime video imaging or stored imaging, telepathology system supports the diagnosis. One of the examples of telepathology innovation and collaboration is to support to patients' benefits for the distance diagnostic service by this change and adaptation. Numerous commercial and academic telecommunications networks have been developed over the years. Telepathology is of great benefit to underserved and rural areas where there is a significant shortage of pathologists. In these areas, not only is there a high demand for diagnostic consultation, but also a need for continuing education and guidance on patient management.
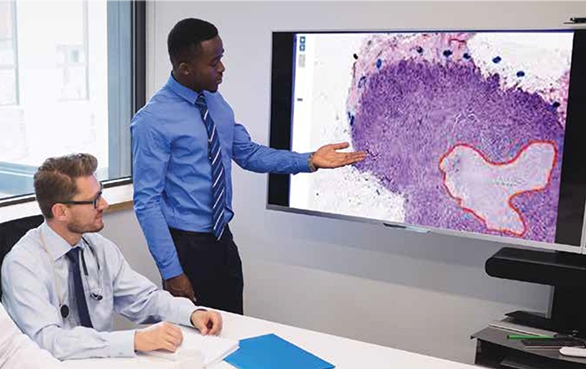
In the recent decades, the implications of digital information technologies to pathology procedure have been spreading out, and the process of conventional pathological diagnostic service is moving with improved accuracy and convenience. Developed countries like Europe, America, Canada, and Japan started using artificial intelligence (AI) in pathology. Meanwhile, developing countries like Bangladesh are using just a digital camera to capture microscopic images and sharing it through online systems. This way they are using telepathology for remote diagnosis to serve their unreached communities.
In developing countries, disease burden is the highest with very limited resources for healthcare; a shortage of pathologists led to delays in diagnosis, sometimes misdiagnoses, and postmortem examinations. The lack of qualified health professionals and adequate facilities are the highest obstacles to overcome in the healthcare delivery throughout Southeast Asia, South Asia, and Africa. There is a worldwide acknowledged shortage of trained pathologists greater than the primary care physicians with an estimation of more than 500,000 people per pathologist in the African continent. Technological innovation and various efforts to fill the human-resource gap in pathology have led to the evolution and expansion of diverse telepathology solutions across the continent. Many platforms have accommodated the options for telepathology in developing and underdeveloped countries in sub-Saharan Africa. A lot of progress has been made to help pathologists collaborate and bridge the gap of pathology service through the pairing of remote facilities with experienced ones. Diagnostics application is the most common use of telepathology in low resource settings along with teaching, education, and quality assurance. Apart from the diagnostic use, the adoption of telepathology in many underdeveloped countries may be a form of two-way communication, locally approachable services with user acceptance, low operational cost, and low risk during disease pandemic. However, telepathology deals with numerous limitations in scaling up and widespread adoption. Two major factors as power supply and highspeed internet, which are extremely lacking in underdeveloped countries for telepathology. The legal barrier of health professionals in delivering care across borders and security concerns related to the confidentiality of medical information on the internet is still unclear. Multiple approaches including operational feasibility are essential to solve these problems.
Bangladesh is one of the developing counties with a critical shortage of health care facilities as well as care professionals. Grameen Communications of Bangladesh has developed a telepathology system as an Information and Communication Technology (ICT) based healthcare service system. Grameen Communications started this telepathology project in 2016 in four different rural and sub-urban hospitals for unreached communities of Bangladesh. In this project, haematological (complete blood count), stool (routine microscopy), and urine (routine microscopy) tests are being provided as some of the telepathological services. Before starting the telepathology service, they ensured basic requirements were met for the successful implementation of the service, such as: 1) Skilled and trained human resource (e.g., pathologists and medical technologists), 2) Telepathology service platform, 3) Internet access, 4) Microscope, and 5) High-resolution camera/smart phone with a structured camera/phone holding frame.
A service team was built comprising of one online pathologist in the city and one laboratory technologist in each remote site. First, the laboratory technologist collects patient’s basic information like name, age sex, address and cell phone number for online registration. Then she/he collects blood sample, prepares slide, takes 6-10 microscopic images of a slide from different significant locations using conventional microscope and digital camera, and uploads the images to the online server of the telepathology system. Finally, the remote pathologist prepares the pathological digital report using telepathology system by image analysis and shares with the laboratory technologist through the online system. By using telepathology system, Grameen communications served 3,000 remote patients.
The COVID-19 pandemic is leading to unprecedented burdens on regional and institutional resources in healthcare facilities globally. The medical systems worldwide are facing unexpected operational challenges and stress to their social infrastructure and healthcare systems. The pathologic diagnoses and integration of histopathological and molecular data are crucial for timely induction of right treatment regimens for even non-COVID-19 patients with serious medical conditions. During public health emergencies like this COVID- 19 pandemic, when the infection risk becomes higher, the remote use of digital pathology enables healthcare systems to keep pathology operations going. The pathologists, their colleagues, and family members are at risk of contamination by a deadly virus. This disruption is causing revolutionary downstream effects to the healthcare delivery system, including essential anatomic pathology services. Workplace transmission events may lead to reductions of laboratory or health personnel due to exposure and/or sickness. If pathologists are unable to be present at their working facilities due to illness, quarantine, or travel restrictions, healthcare system will lose continuous patient care and cause uncertainty of pathological reporting. Several published studies have reported that when the patient care and protecting healthcare personal safety is crucial, the pandemic has found benefit in digital pathology for reviewing and reporting of pathology specimens for ensuring uninterrupted and expert pathology practice. Pathologists have been instructed to work from home during the COVID-19 pandemic like many other professionals.
In this current pandemic situation, the remote telepathology allows healthcare systems to maintain pathology operations during public health emergencies. This situation makes eHealth necessary as it can overcome geographical barriers, increases the number of people served, and provides online diagnosis support for patients. The COVID-19 outbreak is just the latest factor in support of enabling remote review of anatomic pathology images and cases. The trend of using telepathology, whole-slide imaging, and digital pathology systems have been gathering momentum for several years. Powerful economic forces support this trend.
Telepathology systems have appeared as an amazing gift for ensuring effective healthcare service at low costs. And this was actualised only because of the advancement of information technology, specially, the internet. To, mitigate the long-lasting sufferings of developing countries, this ICT-based telepathology system can provide satisfactory diagnosis for the most remote places using internet facilities. Therefore, where pathology services are unavailable and inadequate, a positive attitude in local government, and national and international organisations, especially the scientific bodies, is required.
Implementation challenges of this system include a change in the traditional mindset of patients and physicians. It is not possible to perform all tests by this telepathology system like biochemistry, serology and immunology. The gap of distance pathology service can be reduced using the telepathology system by an online professional pathologist. If the telepathology approach can be scaled up throughout the world, it might contribute to improve healthcare services through proper diagnosis.
Technological innovation is great for many developing countries in critical sectors like health. Telepathology services are minimising the human recourse gap and lead to the development and dissemination of various pathology solutions across the world. A pathologist selects the images to be analysed and study the slides remotely in realtime and deliver immediate analysis. Integration of machine learning and AI is supporting pathologists to make an informed decision. These days, the use of telemedicine has been increasing regularly due to the rapid advancements in ICT. Innovative technologies for digital imaging and telecommunications are changing the way of traditional service delivery process. Infrastructure and experienced skilled staff are the prerequisites for its successful implementation.
In the developing world, telepathology is very essential because of the significant socio-economic differences resulting in urban areas getting better healthcare services while rural and remote areas remain disadvantaged. The telepathology system is an effective and feasible way to provide better treatment during the COVID-19 pandemic.