While a cure has not yet been found, public perception surrounding breast cancer has changed dramatically. Once a disease that women felt ashamed to discuss, breast cancer now has lost much of its stigma, providing the opportunity for politicians and healthcare officials to acknowledge that economic and political considerations bear on the success of breast cancer treatment as much as advances in medical science.
Breast carcinoma is among the most frequent malignant diseases in the world and is the leading cause of death among younger women in developed countries. Currently, 1 in 7 woman in these countries will have the disease in their lifetime (Boyle and Ferlay). Since 1940, the incidence of breast carcinoma has gradually increased at a rate of approximately 1 per cent per year in Western countries (Harris et al.). On the other hand, mortality from breast cancer has declined in countries with organised population-based mammography screening (Smith et al. 2004).
New efficient therapeutic regimes have led to prolonged survival of patients with improved quality of life (Hortobagyi). These interventions have considerably increased the number of breast cancer survivors, and a further increase of 31 per cent is expected from 2005 to 2015 (De Angelis et al.).
Screening, diagnosis, and treatment will place an ever growing burden on the healthcare system, in addition to the psycho-social consequences for the women of coming generations. Obviously, a paradigm shift in understanding the natural history of breast carcinoma is needed to develop new and more efficient preventive, diagnostic, and therapeutic alternatives and break the negative trend.
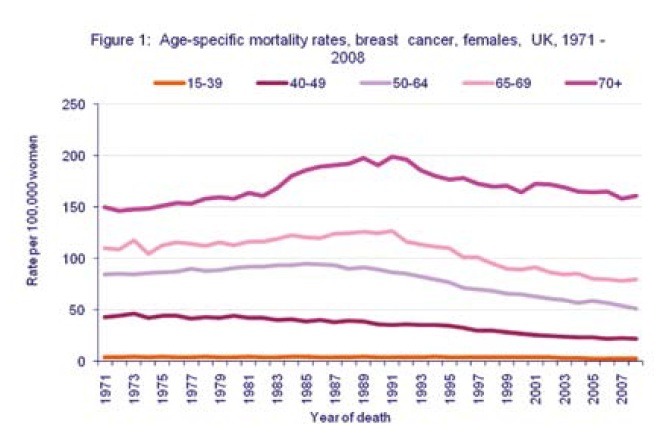
Mortality rates have declined in all age groups since the late 1980s (Figure 1). Between 1989 and 2008, the breast cancer mortality rate fell by 44 per cent in women aged 40-49 years; by 44 per cent in women aged 50-64; by 37 per cent in women aged 65-69; by 39 per cent in women aged 15-39; and by 19 per cent in women over 70. Two major reasons have been attributed to this decline: increased use of screening mammography and greater use and improvements of adjuvant therapies such as hormonal and chemo-therapeutic agents. In UK, breast cancer is the most common cancer accounting for 31 per cent of all cases in women; the next most common cancer in women is lung cancer. So nearly a third of all new cancers in women are breast cancers. It has been estimated that the lifetime risk of developing breast cancer in 2008 is 1 in 1,014 for men and 1 in 8 for women in the UK.
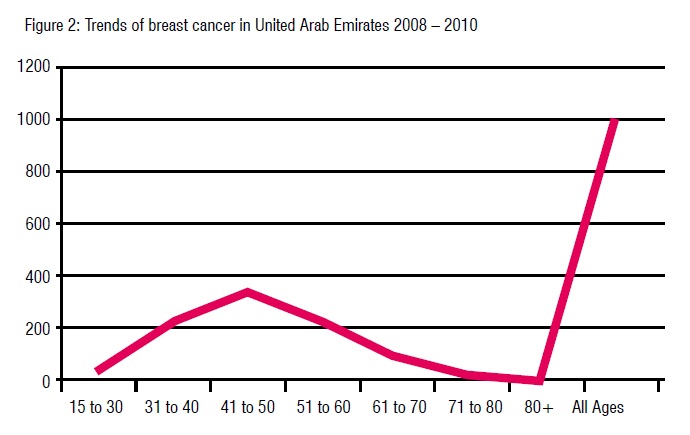
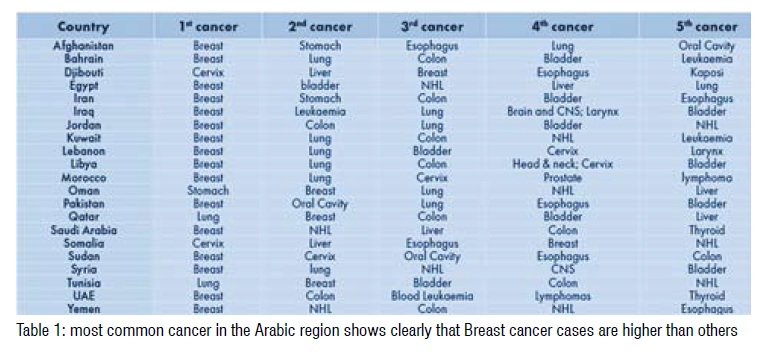
A recent retrospective analysis in UAE showed that breast cancer risk is related to age, with 35 per cent of cases occurring in women aged 40 years and over. Nearly 24 per cent of cases of breast cancer are diagnosed in the 50-69 age groups (Figure 2). According to the World Health Organisation, the occurrence of breast cancer ranks number 1 in most Arabic countries (Table 1). An increase of more than 50 per cent of breast cancer cases has been seen in UAE over the past decade.
Mammary carcinoma has been documented as far back as 6000 BC, but the attempts at treatment can only be considered barbaric. Egyptians treated this cancer by literally burning it out. They would cauterize the mammary glands so painfully that women nearly never came forward when they noticed a lump. Dying of a mammary carcinoma happened to be a much better fate than the treatment of the day as was the case even up until the 18th century.
Mastectomy for breast cancer was performed at least as early as 548 CE, when it was proposed by the court physician Aetios of Amida to Theodora. It was not until doctors achieved greater understanding of the circulatory system in the 17th century that they could link breast cancer's spread to the lymph nodes in the armpit. The French surgeon Jean Louis Petit (1674–1750) and later the Scottish surgeon Benjamin Bell (1749–1806) were the first to remove the lymph nodes, breast tissue, and underlying chest muscle.Their successful work was carried on by Halsted who started performing mastectomies in 1882. Halsted became known for his radical mastectomy, a surgical procedure that remained popular up to the 1970s and was performed on Betty Ford.
By the 19th century, the use of anaesthesia as well as sterilization was brought into the surgical industry which lessened pain and improved the patient's chances of survival and complete recovery. Once this had occurred, not only were mastectomies much more common, but breast reconstruction become possible without putting the patient's life in as much danger as previously.
Since the advent of the modern era radical mastectomy first performed in 1882, great strides have been accomplished over the last century leading to the modified radical mastectomy in the 1980s and to present day breast conserving surgery.
The Halsted radical mastectomy, once considered the ideal cancer operation, no longer has a place in the routine management of patients with breast cancer. This represents a major departure from Halsted's principles of the total resection cancer surgery which was very disfiguring.
Prospective randomized clinical trials in the 1970’s demonstrated no difference in survival between patients treated with modified radical or radical mastectomy. The most influential of the studies refuting the Halsted's principles was the NSABP-BO4 trial. Published results of modern prospective randomized trials comparing conservative surgery with radiotherapy and mastectomy have all shown equivalent survival between the two treatment approaches.
Other studies are ongoing as well to establish the validity of the less-invasive sentinel node biopsy in determining axillary nodal status. Perhaps the most significant change in today's approach to breast cancer is the reliance on well-controlled prospective studies to evaluate outcome and determine the appropriate surgical procedure.
Advances in hormonal therapy have also had a great insight on breast cancer survival. In the 1880s a few physicians reported significant regression of breast cancer tumours following removal of the ovaries. In 1896, George Beatson performed the first bilateral oophorectomy as a breast cancer treatment. In 1966, the receptors for estrogen were identified. With this finding, a target to stop growth of breast cancer cells fueled by estrogen was explored. A few years later, V. Craig Jordan showed that Tamoxifen could prevent breast cancer in rats by binding to the estrogen receptors. In 1977 Tamoxifen was approved by FDA for hormone positive breast cancer.
The Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) overview analysis demonstrated a significant advantage with the addition of Tamoxifen for five years to the adjuvant therapy regimen of women with estrogen receptors positive breast cancer regardless of age.
In 1998 Bernard Fisher reported that Tamoxifen reduced the incidence of breast cancer by 45 per cent in high-risk women; this was the first successful chemoprevention trial in breast cancer.
Treatment with Tamoxifen reduced the risk of death by 14 per cent in women younger than 50 and by 27 per cent in those 50 years of age and older. The late 1990s saw the introduction of a new class of drugs called aromatase inhibitors. These drugs are currently available for hormone positive breast cancer in post menopausal women. Although overall survival has not been reported, time to disease recurrence and time to distant recurrence, and reduction in the incidence of contralateral breast cancer all favor the use of AI’s.
The 1980s saw the discovery of the Cerb2 or Her2/neu gene by Dennis Slamon and others. Approximately 20 per cent of breast cancer patients have her2/neu positive cancer. This is associated with reduced survival and time to relapse. Slamon’s discovery provided an important opportunity to evaluate the concept of targeted cancer therapy and in 1998, Trastuzumab , the first humanized antibody targeting a cancer related gene was approved by the FDA for her2/neu – positive MBC. Eight years later, it was approved in the adjuvant setting. Another drug, Lapatinib; which inhibits the intracellular tyrosine kinase domains of EGFR and her2 receptor was added to the armamentarium of her2 positive breast cancer in the 2008.
Pertuzumab, an anti-HER2 humanized monoclonal antibody that inhibits receptor dimerization, and has a mechanism of action that is complementary to Trastuzumab, has shown encouraging results in recently published clinical trials
Breast cancer is a relatively chemo-sensitive disease and chemotherapy in both the adjuvant and metastatic setting is used widely. Another major contributor to the improvement in breast cancer survival has been the institution of systemic chemotherapy in the adjuvant as well as the metastatic setting since the 1970’s. Randomized trials have addressed many fundamental questions related to adjuvant chemotherapy. The two major trials which had an impact on the care of women with breast cancer and the design of future strategies were the NASBP trial using Melphalan and the trial by Bonnadonna using CMF. CMF quickly became the standard of care for node positive breast cancer. In recent years, anthracycline and taxanes have become the backbones of treatment as many trials incorporating these agents have had a great impact on survival. The new century brought with it the use of antiangiogenic agents to control cancer. This concept dates back to 1971 with the discovery by Judah Falkman that angiogenesis plays a major role in tumor growth and metastases. Bevacizumab, a humanized monoclonal antibody that targets the VEGF became the first antiangiogenic agent approved by the FDA in 2004 for colon cancer. Approved in early 2008 for metastatic breast cancer, its use in the current setting has been revoked by the FDA, though the European Medicines Agency (EMEA) still considers Bevacizumab as a treatment option in certain settings
The most well-publicised breast cancer gene, and the one associated with the highest risk of developing the disease, is BRCA1. Another gene--BRCA2--causes significantly increased risk, as well. All people have these genes; only when humans inherit certain mutated forms do their breast cancer risk increases. According to the American Cancer Society (2009), Women who inherit the mutated version of BRCA1 or BRCA2 have a 57 or 49 percent chance, respectively, of developing breast cancer by age 70. Fortunately, less than 1 percent of the world population carries the harmful versions of these breast cancer genes.
It is in the 1990’s, when Mary Claire King localized the BRCA-1 gene for inherited susceptibility to breast cancer to a specific site on chromosome 17, the BRCA-1 gene was ultimately cloned in 1994. King demonstrated that a single gene on chromosome 17, later known as BRCA1, was responsible for many breast and ovarian cancers—as many as 5-10 per cent of all cases of breast cancer may be hereditary. The identification of two tumor suppressors’ genes BRCA-1 and BCRA-2 has provided great insights into the understanding of breast cancer genetics.
Epidemiological studies have established a set of relatively convincing risk factors for breast cancer such as: family history of breast cancer, possibly due to inherited genetic abnormalities; rapid growth early in life, greater height, higher socio-economic status, and older age. In addition, some probable risk factors are: diet low in fruit and vegetable intake, or high in meat/fat intake, higher alcohol consumption, high post-menopausal body mass index (BMI), and lack of exercise and history of benign breast tumours.
Breast cancer is by far the most frequent cancer among women with an estimated 1.38 million new cancer cases diagnosed in 2008 (23 per cent of all cancers), and ranks second overall (10.9 per cent of all cancers). It is now the most common cancer both in developed and developing regions with around 690,000 new cases estimated in each region, Current World wide Breast Cancer Age-standardized mortality rates is 14.1 per 100,000 population in 2008; while in U.A.E. it is estimated at 10.9/ 100,000 new cases diagnosed per year and an estimated 75 deaths.
With the decline of the Halstead radical mastectomy and a revised theory of metastases, physicians hypothesized about the origins of breast cancer and, during the 1990s, everything ranging from diet, chemical pollution, race, delay in having children, and breastfeeding was up for debate. A recent research has also shown that obesity may increase the risk of developing breast cancer as well. Despite this uncertainty, there are still advances in the treatments for breast cancer; with breast cancer rates and deaths remaining high until 1995. The improvements in chemotherapy, radiation, hormonal treatments, mammography, and surgery helped move breast cancer from an urgent disease to a chronic condition. Today, advances in molecular and genetic sciences are creating novel therapeutic strategies that give women not only hope but also more choices about their bodies. There are some studies in their initial stage are currently ongoing using the concept towards creating an anti breast cancer vaccine.
Breast cancer is a complex, diverse, and so subtly connected to genetic and environmental variables making a cure can often seem impossible. While a cure still has to be found, public perception has changed in recent years. Once a disease that women were concealing, breast cancer now has lost much of its stigma and women are open to discussing their disease and seek treatment, providing the healthcare officials with an opportunity to acknowledge that economic and political considerations bear on the success of breast cancer treatment as much as advances in medical science.