Care providers must consider some key factors they need to balance for effective implementation of patient-centric modalities.
In recent times there has been a trend towards adoption of patient-centric modalities as a cost-effective way. These modalities address the needs of various groups of the population, including the ageing population segment, a large percentage of which are affected by chronic conditions that are the leading causes of illness, disability and death. Patient-centric modalities aim for effective integration of technologies, information and tools to address patient care needs and to enable comprehensive treatment, and close physician guidance and coordination. Ideally, in this environment, physicians will be able to make critical decisions for their patients with complete and relevant information, real-time input from online clinical decision tools and access to electronic health records.
The current health system and technology and / or disease-centric approaches to the design of medical devices and therapies offer, in most cases, fragmented care that is inconsistent with the scope of needs described above. These needs can only be addressed effectively by a patient-centric view of medicine, technology and regulations.
How it all plays together
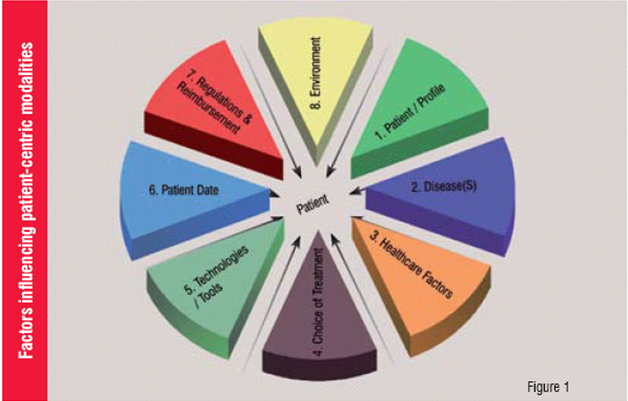
The typical factors that we must balance for effective implementation of patient modalities are: patient / profile, disease, healthcare factors, choice of treatments, available technologies and specialised tools, patient data, regulations & reimbursement and environment (Figure 1).
Intangible factors
The factors listed above plus other intangibles such as the quality of the relationship between the patient and the healthcare provider are closely linked and must be balanced to ensure a successful outcome.
Positive relationship
A positive relationship between the care provider and the patient can lead to full understanding of the patient profile. The patient profile involves looking at a variety of factors that provide the full picture of the patient. They include elements such as gender, age, weight, height, overall health, dietary preferences, genetics, background and ethnic characteristics, lifestyle, personality, religious beliefs, psychological profile and mental health. The understanding of the patient profile together with the patient's views and priorities is the first step in developing a successful patient-centric modality.
Understanding the disease
The second set of factors requires an understanding of the stage of the disease or diseases, for instance, is it an acute or a chronic condition? Is it a single or multiple conditions? Do we understand the trade-offs of therapies, monitoring and sample requirements, e.g. type, frequency, quantity and how these parameters affect the patient and the selection of any available treatments. This can be accomplished through a systematic series of examinations and gathering of data and correlation with the medical history of patient. One opportunity in this area is the education of the patient about the disease. The level of education that the patient has about his or her condition and the awareness of the progress and constraints faced by the provider will enhance the chances of a successful outcome.
Healthcare factors
The third set of factors is designated as the healthcare factor. The elements connected to healthcare are mainly driven by the care provider and the provider preferences, level of care, availability and affordability of treatment, quality of provider services, socialised medicine or for profit model, provider policies and insurance coverage.
The three set of factors above can help narrow down the treatment plan or choice of treatments, including deciding among traditional, non-traditional and holistic medicine. Also, there is an array of alternatives available depending upon the condition being treated. In recent times, there has been an increased attention to therapies combined with dietary practices.
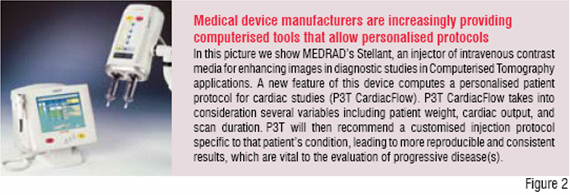
Along with the above, we have a choice of technologies and tools that allow deeper investigation, going from laboratory testing to imaging to genomics. The promise of genomics is that we would evolve into a truly personalised medicine by including the patient's genotype and levels of gene expression. This allows precise tailoring of the treatment to the individual. In the area of medical devices, we are already observing a shift towards providing the physician with the tools to personalise treatments. Many companies are using this as a way to differentiate their products. Figure 2 illustrates a contrast injector used to enhance imaging procedures. This device allows entering a patient's physiologic parameters to recommend personalised settings for delivering a customised contrast protocol (volume and flow rate) to a specific patient.
The resulting patient data offers challenges of its own. The collection, storage, retrieval and analysis of the data coupled with the logistics of managing the information itself has opened up a series of opportunities for a new technical discipline, Healthcare IT. Other factors include ensuring portability, data accuracy and integrity, plus data security and privacy issues.
Additional considerations include the regulatory and reimbursement environment. In an ideal world, these two factors would be considered non-issues. However, depending on the conditions being treated and the type of therapy being pursued, they may pose major constraints on the patient and the provider. Last but not least, the environment around the patient plays a crucial role, for instance the hospital versus home care setting; and urban versus rural setting. The quality of patient's life, occupation, living conditions, support networks, all influence the outcome of the treatment.
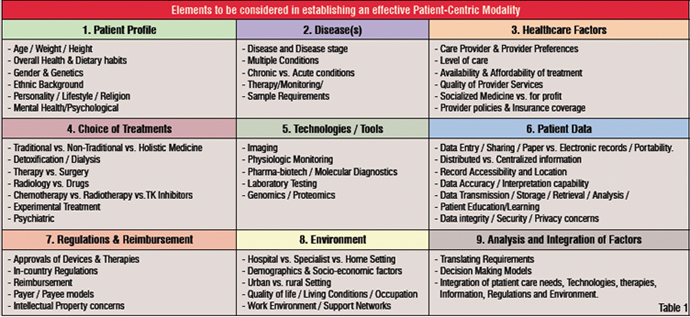
Once all the above mentioned are considered, one is ready to narrow down the development of a treatment plan, which would include the type of therapy and testing, observation, periodic assessment and rationale for plan updates and possibly referral and follow-up. Table 1 illustrates the aggregate of elements that come into play. We can see that the analysis and integration of factors can become a complex decision requiring formal tools to ensure an effective patient-centric therapy.
Opportunities and challenges
Opportunities to facilitate the evolution towards patient-centric modalities include a strategic and behavioural shift from the pharmaceutical industry since they currently develop and commercialise drugs that are targeted to broad segments of the population as opposed to targeting designated sub-populations. The medical device industry also needs to increase its efforts in developing diagnostic tests that would enhance the definition of those sub-populations.
Also, the regulatory environment in most countries fosters above practices by requiring expensive and lengthy clinical trials that add to drug development costs. A concept being proposed in recent times is to allow for expedited approvals of drugs that have demonstrated effectiveness to a smaller sub-set of the population, e.g. by targeting a population segment with a common genetic characteristic and require testing for that characteristic prior to administering the drug.
Another opportunity is related to the current training of physicians and what is expected from them is acceptable
behaviour when it comes to treating a disease. Traditional methods can be compared with trial and error-repair strategies, as opposed to a carefully crafted treatment plan.
On the healthcare system side, we are challenged with systems that establish providers' compensation plans that are largely focussed on completing procedures and prescribing medications as opposed to early disease detection and prevention.
In terms of patient data, some of the upcoming challenges in this area require adopting a different paradigm. Traditional patient records, even in electronic format, organise the patient history from the provider's perspective in a chronological sequence of events. However, they do not support physician-patient interaction or ease communication with the patient. For the next generation of data systems to be fully supportive of patient-centred modalities, they are expected to look at presenting the data in a way that the patient can get the full educational benefit from his / her own health assessment and affect to his or her behaviour. Further, this data can also be combined in a way to facilitate decision-making and help narrow down choices of treatments.
Additional opportunities exist in the use of systems engineering techniques for translating individual patient and situation requirements into actual therapy or modality and implementation maps. To establish objective decision-making, these models optimise the integration of patient care needs, technology and tools, therapy alternatives, information requirements, regulatory constraints and environmental factors.
Conclusion
Patient-centric modalities improve the effectiveness of our healthcare systems thereby benefiting patients. While the extent of changes required at industry, governance legislation, provider and consumer levels are numerous and profound, the shift towards patient-centric modalities has already begun and is expected to accelerate in the coming years.
Acknowledgements
Many thanks to Larry Kopyta, Tito Aldape, Anthony Emerick and Linda Rachul-Rymniak from MEDRAD Inc. that reviewed the draft and provided valuable inputs to this manuscript. Many thanks also to Al DiRienzo, Susan Alpert, Javad Seyedzadeh and Tom Taylor, for their valuable comments and insight during the forum discussion on Patient-Centric Modalities. "Translating Requirements and Integrating Technology" at Frost & Sullivan's Medical Device Conference in March 2006. These early discussions helped establish the groundwork for this article.
Julio A Reategui is Director of RA / QA and Compliance, Asia-Pacific, at MEDRAD, Inc. He has over 25 years of experience developing and commercialising clinical, laboratory and field instrumentation and disposable devices for the medical industry, life and analytical sciences, and environmental monitoring applications , worldwide. He has also authored / co-authored seven patents and over 15 technical publications.